As schools, offices, businesses and e-discovery review centers reopen, facilities managers are looking at elevated risk of coronavirus transmission
2 October 2020 (Amsterdam, The Netherlands) – There is a growing consensus that one of the primary ways the novel coronavirus spreads is through the air. You can find numerous studies and reports on the web but there are two very good ones I highly recommend: a piece in Scientific American which you can read by clicking here, and a piece in Environmental International which you can read by clicking here.
With a hat tip to the founder of The Project Counsel Group, Greg Bufithis (now retired) for providing those links. For those interested, he has posted numerous pieces on COVID-19 which you can read here. He has a detailed piece in progress on what’s become known as “long-COVID” … more and more people suffering symptoms of the virus for longer than the WHO originally predicted or expected … and its affect on our restless distraction that stems not just from not knowing when it will all end, but also from not knowing what that end will look like, or what might come next. We’ll try to snag a copy.
As e-discovery review centers have begun to slowly reopen based on our U.S. and European job postings … by staffing agency/legal vendors sites plus law firm sites … I began to examine the whole issue of airborne spread COVID. This week I was able to attend two pretty comprehensive Zoom chats … one by Science magazine and one by the Building Engineering Controls Program at the U.S. Centers for Disease Control and Prevention (CDS). I also was able to access some relevant material on Quartz to which we have a subscription.
NOTE: There has been a lot of flack in the U.S. over the Trump Administration pretty much gutting the CDS but I can happily report many staffers in the CDS are just soldiering on.

The articles I noted above are pretty good but just a few points from the Science Zoom chat:
- Inhaling small airborne droplets is probable ranked as a third route of COVID infection, in addition to more widely recognized transmission via larger respiratory droplets and direct contact with infected people or contaminated surfaces.
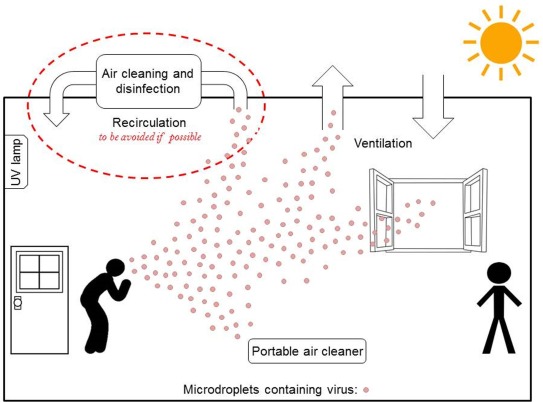
- While uncertainties remain regarding the relative contributions of the different transmission pathways, existing evidence is sufficiently strong to warrant engineering controls targeting airborne transmission as part of an overall strategy to limit infection risk indoors. Appropriate building engineering controls include sufficient and effective ventilation, possibly enhanced by particle filtration and air disinfection, avoiding air recirculation and avoiding overcrowding.
- While this evidence of airborne COVID transmission is incomplete at present, more and more cases are arising and as we enter winter in many parts of the world the threat is serious as the COVID-19 pandemic continues.
- Infection control specialists are being brought into office spaces and testing the relative contribution of airborne transmission compared to the other transmission modes (“direct contact” and “droplets found on a surface”) and multiple studies have provided strong evidence for both indoor airborne transmission of viruses, particularly in crowded, poorly ventilated environments, and surface contamination.

And a few points from the Building Engineering Controls Program Zoom chat (recorded and from distributed materials):
- Ventilation should be recognised as a means to reduce airborne transmission. Ventilation is the process of providing outdoor air to a space or building by natural or mechanical means. It controls how quickly room air is removed and replaced over a period of time. In some cases, it is necessary to remove pollution from outdoor air before bringing it into a building, by using adequate filtration systems. Ventilation plays a critical role in removing exhaled virus-laden air, thus lowering the overall concentration and therefore any subsequent dose inhaled by the occupants.
- Appropriate distribution of ventilation (e.g. placement of supply and exhaust vents) ensures that adequate dilution is achieved where and when needed, avoiding the build-up of viral contamination. The central guiding principle is to replace contaminated air with clean air, but sometimes local barriers to this process may occur, e.g. where partitions are used in offices.
- Hospital facilities normally have sophisticated mechanical ventilation systems. But offices and normal public buildings and other shared spaces have a hodgepodge of ventilation systems that can range from purpose-designed mechanical systems to simply relying on open doors and windows. In most of these environments, ventilation rates are significantly lower than in hospitals for various reasons, including limiting airflows for energy and cost savings, so before planning to reopen your facility you must do a ventilation system audit.
- That is the danger: as “stay-at-home” lockdown measures are gradually relaxed, much of the population will return to spending increasing amounts of time in inadequately ventilated workplaces, offices, and other public buildings, where they may be exposed to a risk of acquiring viral infections by inhalation.
- Ventilation rates can be increased by system modifications. In a mechanically ventilated building, ventilation air is typically provided by a heating, ventilating and air conditioning (HVAC) system. Sometimes, ventilation air is provided by dedicated fans or outdoor air units. HVAC system control strategies can usually be modified to increase ventilation to a certain extent in the occupied zones, with relatively little additional cost, to reduce the risks of airborne transmission between occupants.
- However, this is not via a simple “flick of a switch”, as HVAC systems are complex and usually designed for individual buildings within standard specific operating parameters. Many requirements need to be considered apart from the ventilation rate, including control of temperature, relative humidity, air flow distribution and direction.
- If ventilation is provided using windows openings (aeration) or other means (fixed openings, e.g., natural ventilation), an estimation of the possible outdoor flow rate can be made by an environmental engineer.
- For naturally ventilated public buildings, particularly in cold climates, other challenges will arise, but these can also be addressed in order to reduce the risk of airborne infection transmission.
- The recirculation of air is a measure for saving energy, but care must be taken, as it can transport airborne contaminants (including infectious viruses) from one space and distribute them to other spaces connected to the same system, potentially increasing the risk of airborne infection in areas that otherwise would not have been contaminated.
- Particulate filters and disinfection equipment in recirculated air streams can reduce this risk, but they need to be purposely designed to control risk of airborne infection and need regular service to maintain their effectiveness. Many systems are designed for filters that are intended to remove larger particles that may affect the functioning of equipment and that are not effective at removing small, sub micrometre or micrometre size particles associated with adverse health effects.
- Following the above considerations, during an epidemic, including the current COVID-19 pandemic, air should not be recirculated as far as practically possible, to avoid the dissemination of virus-laden particles throughout the indoor environment For central air handling units at a building level or serving multiple zones, recirculation should be avoided, and the system operated on 100% outdoor air (OA) if possible.
- In environments where it is difficult to improve ventilation, the addition of local air cleaning or disinfection devices, such as germicidal ultraviolet (GUV, or UVGI – ultraviolet germicidal irradiation) may offer benefits. Under laboratory conditions GUV has been shown to be effective against a suite of microorganisms including coronaviruses.
- Portable consumer air cleaning devices may be beneficial in smaller rooms, although it should be recognised that such devices must be appropriately sized for the space. There is wide variation in performance of air cleaners depending on air cleaner design and size of room in which it is used.
- Minimise the number of people within the same indoor environment in an epidemic. This measure is self-explanatory in the context of the need to lower the concentration of airborne virus-carrying particles, and reduce the number of people who can be exposed at any time. There is no one specific value for a number of people who could share the same space during pandemics, and this measure should be considered in conjunction with the engineering measures discussed above, and particularly in relation to the ventilation parameters of the space.
- Although the physical distance required to avoid transmission through direct contact dictates the requirements for the floor area per person, the rate of ventilation provided and the efficiency of ventilation are the parameters that control the concentration of virus-laden microdroplets in the air exhaled by the occupants, and will guide decisions on safe occupancy numbers.
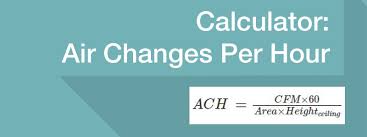
One interesting bit in the Zoom chat plus the Quartz materials was that facilities managers are looking at one particular metric to gauge whether there’s an elevated risk of coronavirus transmission: air changes per hour (ACH). Just a few quick points:
Air changes per hour (also known as “outdoor air changes per hour”) is pretty easy to understand—it’s the rate at which the air in a space is completely recycled. The higher the ACH, the more frequently air is cycled through, reducing the risk that a person in that space will inhale viral particles and get infected.
So far there’s no official recommendation on the ideal ACH to dramatically reduce the risk of transmitting COVID-19. That’s because it depends in part on numbers we don’t know yet, like how many viral particles an infected person spreads, or how many can make an exposed person sick. For a deeper look click here. For now, most experts suggest at least 3 ACH, and ideally 6 ACH, though these numbers haven’t been officially adopted by organizations that set ventilation guidelines
Here’s are estimated ACH in spaces where you might find yourself, as laid out in the Quartz material:
- Home: 0.35 ACH
- Home with one window open: 0.8-1.3 ACH
- School: 3 ACH is the minimum recommended; 1.5 ACH is the reality for most schools
- Office: 6-8 ACH recommended
- New York City subway: 18 ACH
- Parked car with a window open: 6.5 ACH
- Car moving up to 72 mph with ventilation system off: less than 6.6 ACH
- Airplane: 10-20 ACH
- Laboratory: 4-8 ACH
- Patient room at a dentist’s office: 6-12 ACH
- Medical facility with patients affected by airborne diseases: 6 ACH minimum, 12 ACH recommended for new constructions
One engineer on the Zoom chat noted that “actual outdoor air flow rates in most buildings are lower than the total equivalent air change rates being recommended for Covid-19 airborne risk management.” In other words, you can’t rely on the numbers above as a perfect metric to gauge your risk of catching COVID-19.
Figuring out air changes per hour in your space is possible, if a little complicated. You’ll need to know the volume of air in your space (width x length x height of the ceilings), and the amount of outdoor air flowing in (measured in cubic feet per minute). That last metric is something you can find out if you have an air purifier or an HVAC system. For a helpful video:
Or you can just use this handy calculator.
And ACH is not the only metric that can give you a sense of whether a space is well ventilated. The outdoor air flow rate – how fast outdoor air is moving into a space – is also important to consider.
Plus, ACH has limitations to its usefulness. In houses, the amount of contaminated air varies based on how many people are home. In office spaces (maybe some with high ceilings) only the bottom space is occupied, so if air change rate is used at all, it should probably be based on a reasonable estimate of the occupied volume – for example a zone extending to 10 feet above floor level. This really underscores the need for recommendations for changes to building operations to be implemented by competent professionals.
Bottom line: all the points made above will increase air changes per hour in your space.

For the Science magazine presenters, until effective pharmacological treatments or vaccines (all were cautious on when those could be developed, even whether they could be developed) so as to reduce the effective reproductive number to less than 1.0 and stop the ongoing COVID-19 pandemic, enhanced ventilation will be a key element in limiting the spread of COVID-19.
For the engineering Zoom, these were the key ventilation-associated recommendations:
- Building managers and infection control teams have engineering controls available to effectively control and reduce the risks of airborne infection – and COVID-19 clearly has the potential and is likely to be causing some infections by this route. Get some qualified environmental engineers on board.
- You can increase the existing ventilation rates (outdoor air change rate) and enhance ventilation effectiveness using existing systems.
- You must eliminate any air-recirculation within the ventilation system so as to just supply fresh (outdoor) air.
- Supplement existing ventilation with portable air cleaners (with mechanical filtration systems to capture the airborne microdroplets), where there are areas of known air stagnation (which are not well-ventilated with the existing system), or isolate high patient exhaled airborne viral loads (e.g. on COVID-19 cohort patient bays or wards). Adequate replacement of the filters in the air cleaners and their maintenance is crucial.
- Avoid over-crowding
If implemented correctly, these recommended building-related measures will lower the overall environmental concentrations of airborne pathogens and thus will reduce the spread of infection by the airborne route. Together with other guidance on minimising the risk of contact and droplet transmission (through hand-washing, cleaning of hand-touch sites, and the appropriate use of PPE), these ventilation-related interventions will reduce the airborne infection rates not just for COVID-19 but also for other airborne infectious agents.
While much of the focus has been on case finding, isolation and quarantine, social distancing and hand hygiene, both groups emphasised that a parallel reduction in airborne transmission using such engineering controls will further protect your workforce.